All published articles of this journal are available on ScienceDirect.
Impact of Health Information Technology Tools on Patient Safety in the Indian Healthcare Industry
Abstract
An aging population, increasing pollution, and people's lethargic lifestyles are some of the main reasons behind the growth of the healthcare sector. Indian entrepreneurs and researchers recognize this growth, opportunity, and the provision of medical services in different ways. The idea of using cloud-based services via the world wide web, networked systems, etc., in healthcare is known as Health Information Technology (HIT). It primarily uses patient-related electronic medical records, information, and data to provide treatment and services more effectively. The various challenges and issues related to the use of information technology include the unavailability of internet facilities in all regions, the lack of policies, guidelines, standards, and the lack of adequate infrastructure and educated staff members. Developing policies, standards, and guidelines to maintain quality, increasing government funding to improve current infrastructure, and purchasing and installing the appropriate technology based on current healthcare IT-related situations and challenges are some of the recommendations to be made in the existing infrastructure of the healthcare industry. HITs are crucial to maintaining a better healthcare system since they affect overall hospital performance and the quality of health information. This research is not focused on the relationship between HITs, hospital performance and health information quality. It highlights the significance of investing more in HITs and the quality of health information in the healthcare sector, with the predicted outcomes being an increase in productivity, performance leveraging, and mistake reduction.
1. INTRODUCTION
India is at the top of the list worldwide in terms of the origin of medicine and health sciences.India shares the ultimate healthcare links with ancient medicine since it was founded around 500 BC by Dhanwantari, the god of Hindu medicine [1]. Traditional and unconventional medical systems, such as Ayurveda, yoga, naturopathy, Unani, Siddha, sowa-rigpa, and homoeopathy, are available (AYUSH). The six Indian traditional healthcare systems are listed above.
Ayurveda, the conventional Indian system of holistic medicine, is thought to have originated from the ultimate source of Atharvaveda, one of the four Vedas. Ayurveda applies the Thridhosha concept of ailment. Thridhosha describes 3 doshas, or biological elements, which can be connected to a patient's health: Vata (wind), Pitta (gall), and Kapha (mucus). The ailment is defined as a disturbance withinside the equilibrium of the 3 doshas, an idea much like the concept recommended with the aid of using Greek medicine. The history of human evolution is evidence of the fact that humans have always struggled to survive, and in most cases, Darwin's concept of survival of the fittest applies [2]. As with this testimony, it is natural to think that people living an increasingly complex professional and personal life tend to be involved in exaggerated goals and role demands.
The use of tools, machines, technologies, features, systems, procedures, or organisations to execute or resolve particular features is referred to as technology. Information technology is the study of how to process information using technology. On the other side, medical information technology refers to the thorough management of health data across computerised systems and ensures communications between customers, providers, governments, quality agencies, and insurance firms. Health information technology is acknowledged as the most promising tool for enhancing the general level of quality, safety, and efficiency of medical systems, as well as for enhancing widespread and consistent use of HIT quality of care, preventing medical malpractice, lowering medical costs, increasing access to affordable care, and reducing administrative burdens. mHealth is the development and usage of mobile applications for the health and well-being of the community. As mobile phones are portable, accessible everywhere, and being used by almost the majority of our population, irrespective of age, mHealth is blooming.
The main purpose of this paper is to understand the various factors of information technology, to understand aspects of the medical field, and to analyse the importance of information technology in the rapidly growing digital age where medical services play a significant role.
The remainder of this paper is organized as follows: A literature survey related to this work is given in Section 2. Section 3, and 4 narrates the background and origin of HIT, and barriers to the adoption of HIT, respectively. The necessity of HIT in India is vividly explained in Section 5, whereas, section 6 elaborates the HIT in the present. ICT and HIT-based health platforms in India are illustrated in Section 7. HIT in the era of Covid is given in section 8. The conclusion and planned future research activity are given in Section 9.
2. LITERATURE REVIEW
According to Digital Health Market, the healthcare market, in terms of the usage of digital help and assistance, has crossed the budget of $145 million by the year 2021 and is expected to grow to more than $430 billion by 2030 and will be sharing a Compound Annual Growth Rate (CAGR) of 16.9% [3]. In addition, healthcare professionals, patients, doctors, third-party providers, and other healthcare supporters are increasingly seen to be dependent on the use of electronic support and technology in terms of data collection, analysis, prognosis, report reviews, disease prediction, and many more factors that are easily neglected by human eyes due to their minor yet significant contribution. In recent years, it has been observed that amazing results of technology and information communication have reduced human error and are saving the valuable time of patients and researchers with the help of early detection, ease of analysis using various machine learning techniques, the discovery of various medicines or treatments, and improvement in existing methods of healthcare. Information and communication technology, or simply ICT, is changing the implementation of healthcare services in rural areas of India as well. Many government and private hospitals, organizations, and communities are promoting and providing the technological and latest facilities to the poor people and thus leading to an improvised patient-doctor relationship, better clinical governance, and patient satisfaction.
Healthcare is such a domain in today’s world where one cannot afford to neglect their health-related issues, even if it is minor or negligible, because we are living in an era where a situation like COVID-19 has been emerged and has no right remedy besides the vaccination, however, that may not keep one absolutely away from the virus as it is a vaccine despite everything and now no longer an everlasting solution. The interconnection of healthcare and technology generation may be quite evidently visible these days, keeping in view that everyone around us is concerned about their fitness, and to keep track of that, they monitor it wisely using smart technology. For instance, if a person is in a dilemma because his blood glucose level (BGL) is low, he may not visit the health practitioner immediately, however, he will take a look at the BGL with the aid of domestic usage of his smartphone or any smart device, and right here we can take a look that human beings are impartial in their fitness and now no longer are depending on the healthcare experts in small fitness-associated issues.
A few decades back, it was observed that the number of hospitals owned with the aid of using the authority or person becomes much less than the number of sufferers to satisfy their desires with the best healthcare services. However, with inside the state-of-the-art surveys, recruitment of knowledgeable people in the clinics, hospitals, technicians, and other professionals involved in healthcare is carried out even in some of the rural regions lately. The local boom had a surprisingly good solution, as regulations and standards were applied with the help of various state-owned enterprises and local direct government agents.
3. BACKGROUND AND ORIGIN OF HIT
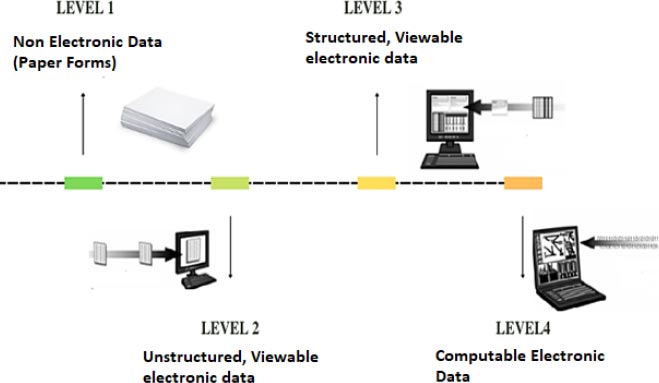
Ayurveda is called the coronary heart of Indian medication and science. It is one of the origins of medicines and surgeries in the Indian sub-continent in the past, at about 1500 BC. Atharvedha, known as the backbone of the Indian Civilization, contains various formulations that are used for treatments and surgeries of different diseases. Until the medieval ages, Ayurveda was probably the only system available to meet people`s health needs in the Indian subcontinent. It enjoyed the indisputable sponsorship and support of the people and their rulers. This era can be regarded as the golden age of Ayurveda, as most of the great visions, dissertations, formulation of work related to the operation, and various directions were revealed. The arrival of British in the country led to arise of various political issues and degradation in the acceptance of Ayurveda because the British initiated the consumption of Allopathy and influenced the Indian people too. After India's independence in 1947, the movement to revitalize the traditional healthcare system gained momentum. This system has been officially recognized and has become part of the National Health Network for providing medical care to national citizens. The Indian government has launched numerous schemes and policies to improve Ayurveda's status as one of the most important health systems essential in providing the country's primary health care. However, simultaneously, a number of schools, colleges, and research institutes were introduced in the country, focusing on the medical domain and building a keen interest in the public and students regarding the usage of Ayurveda. Later, the adoption of computerized techniques was seen in which the implementation of HER (digital version of patient’s health record) played a key role as it is one of the major tools for improvising the quality, safety, and efficiency of healthcare data. In the 1920s, the first-ever health information management emerged by creating a system where professionals could document the patient’s details in digital format. The Association of Record Librarians of North America was created by the American College of Surgeons to standardise this (ARLNA). Later on, further versions of EHR and healthcare management systems were implemented using the HIT wherever possible by the clinicians, doctors, professionals, vendors, and other people involved in this domain (Fig. 1).
4. BARRIERS TO HEALTH INFORMATION TECHNOLOGY ADOPTION
Building a health information system infrastructure is difficult in terms of many parameters like time, money, knowledge, internet, etc. [2]. Adopting HIT varies from developed countries to developing countries for the above said parameters.
Inadequate Infrastructure- Most developing countries do not spend more money on building healthcare systems or buying efficient systems, software, hardware, etc. Strong infrastructures are required for strong healthcare systems to deliver quality healthcare services to the public.
4.1. Poor Internet Availability
Internet plays a crucial role in any informatics system for sharing and exchanging it effectively. It is difficult to achieve the best healthcare services without proper internet facilities.
4.2. Lack of Professionals
Any new technology requires the usage of qualified and trained professionals in order to operate or manage the information system. When we budget for professional development, we have to spend a lot of money on hiring a resource person and acquiring new technological tools. Therefore, training involves both money and time.
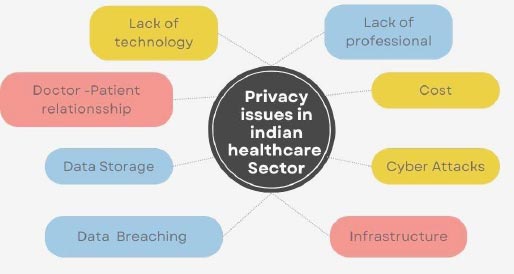
4.3. Social and Cultural Barriers
The expansion of the health care system is hampered by considerable social and cultural barriers, such as the digital divide and e-readiness, due to participants' lack of interest, apprehension, and lack of desire to adopt and use new technology. People are more attached to their traditional approach and daily routine, making the transition to a digital health information system problematic. Organizational Barriers: Businesses are reluctant to invest in new technologies because there is a lack of supporting data, such as surveys or proof models of improved outcomes, and because the traditional approach is convenient (Fig. 2).

5. NEED FOR HEALTH INFORMATION TECHNOLOGY IN INDIA
The broad advancements in technology, education, healthcare, science, manufacturing, and engineering have come a long way and are still going on. It’s a process that is never going to settle down at any stage because the demands of people are increasing day by day. As we are entering a world where humans are becoming fitness conscious and are continuously hustling to stay fit and healthy, but at the same time, we are ignoring the fact that not only healthy food and diet, regular health check-ups, and exercises are necessary but also, keeping track of their complete healthy is equally important. Medical information technology is the use of innovative technologies discovered in medicine or applying the technology launched related to the information or data on healthcare information. Traditionally, healthcare professionals, clinicians, and health insurers used to keep paper records for collecting, maintaining, using and storing patient information and this would lead to errors in billing, research, and the leaking of unwanted data. However, due to digitization, people have started working remotely on their work, and so is happening in the heathcare sector as well. This is leading to the demand for information technology to overcome limitations and provide quality services with utmost accuracy within a short duration. Healthcare requires health monitoring of the public, delivery of quality services, medical practices, etc., and all of these depend on the healthcare management and supply of information technology ultimately for the faster and easy delivery of services. Health information technology helps medical practices access accurate and practical data that can be easily customized to meet specific medical needs, allows access to patient’s EHR and make fast decisions, improved decisions leading to less number health- risks, healthcare management systems used for scheduling appointment, insurance verification, billing, etc. Furthermore, with the help of information technology adoption, the paperwork will be reduced, leading to less time consumption for prediction and diagnosis. Below mentioned are some of the advantages that take place when information technology is implemented in healthcare:
● Accurate and thorough statistics
● Individualized treatment and care programmes for the patients
● Better and quicker communication between patients and healthcare professionals
● The organized and secure patient scientific records
● Simple access to patient records through a crucial database
● As accurate codes are chosen, and valid scientific claims are submitted, prices will decrease.
All of these factors are the reasons that clearly tell us that Indian healthcare needs to have proper information technology and management in order to accomplish the needs of the populace satisfactorily.
5.1. Health Monitoring Systems for Common Health Issues
According to the information provided, in 2050, India will make up 22% of the global population. This is among the most crucial justifications for ensuring that health and assistance services are properly planned for and delivered. Since chronic illnesses and their accompanying side effects can lead patients to behave quite differently depending on their age, seniors require a lot more diverse therapy. Other factors to take into account include low income or insurance coverage, restricted mobility, disability, a rural or distant location, and a negative self of ageing [4-6]. Consequently, eHealth (electronic health services) and mHealth (mobile health services) are evolving into crucial elements of healthcare. The terms “eHealth” and “mHealth” refer to a broad range of healthcare services, including text message reminders for patients to take their drugs as well as electronic prescribing and access to medical information. As a result, mHealth and eHealth are growing in significance in the delivery of healthcare [7].
5.2. Chronic Diseases Management
A considerable amount of attention has been paid in recent years to encouraging “self-management” among those who have chronic diseases. Due to their heightened knowledge of their illness and way of life, patients with chronic conditions typically experience better health outcomes and use less healthcare resources [8]. However, it's critical to address the issue of harmful behaviours among those who lack adequate self-management abilities. This may be avoided by making lifestyle changes and managing chronic diseases in a self-directed manner. It is crucial to provide patients with the tools they need to actively manage their health, with an emphasis on total physical well-being. This calls for creative solutions to improve current healthcare procedures, such as improving medical care and encouraging significant behavioural changes [9, 10].
5.3. Anxiety and Depression
Personal Anxiety and Depression Tracking and Intervention: Due to their ability to consistently collect data on physiology and behaviour and to also deliver effective responses without the use of up limited clinical resources, mobile devices can offer a wide scope of solutions for psychiatric patients [11]. Mobile mental health applications commonly gather context information and integrate it into a clinical diagnosis model to identify the patient's mental health status [12]. The following phase suggests actions to help the user overcome psychological challenges (e.g., Being outcastes from the society).
5.4. Older People's use of eHealth and mHealth
The demands of elderly persons specifically must be taken into consideration when designing digital health services. The main difficulties with eHealth systems' operation include small screens, small text, and a lack of an age-appropriate user interface. The use of mHealth is, however, impacted by other age-related hurdles. These include having limited or restricted money, not being aware to use mHealth and the high expense of new technologies. Mobile technologies are too challenging to utilise. New information and warnings can be overwhelming for seniors. To sum up, it is crucial to incorporate elements like voice feedback, a large font size, and a customizable notification system when creating eHealth solutions for seniors so they may interact with the platform that suits them best. The prevalence of chronic diseases in the community is reduced, and their identification and successful management are influenced by raising this awareness [5, 13-15]
5.5. Mobile Sensing for COVID-19
Mobile microphones have the capability to capture various sounds such as speech, breath, and sigh, which can be utilized for the identification of individual COVID-19 cases [16] and the detection of lung disorders [17]. Brown et al. [18] proposed techniques to identify diagnostic markers of COVID-19 in speech and coughs, enabling differentiation between COVID-19 and other viral illnesses. They employed a three-channel neural network that leveraged data from the COVID-19 Sounds App, encompassing coughs, breathing, and voice recordings, to accurately identify COVID-19 infections. Apart from audio-based diagnostic tools, innovative wearable sensors have emerged as a means of continuous monitoring of subtle indicators that could potentially signify the presence of illnesses [19].
6. CLASSIFICATION OF HEALTH INFORMATION TECHNOLOGY IN THE PRESENT
In current global health scenarios, Information and Communication Technology (ICT) in the form of Health Information Technology (HIT) applications is recognized as a transformative force to improve the delivery of health services in India and the performance efficiency of hospitals as a whole. India's healthcare industry is growing at a tremendous rate due to its coverage, increased services, and increased spending from public and private players. There are various factors that play a decisive role in its implementation and demand in the public. Some are as follows:
● Electronic Health Records (EHRs) are extensive computerised libraries that logically arrange patient or population-specific health-related data. They make it possible for digital records to be shared and stored among numerous healthcare providers. EHRs contain a variety of data, including demographics, medical history, information on medications and allergies, immunisation records, laboratory test results, radiographic pictures, vital signs, and personal details like age and weight [20].
● Telemedicine: The goals and activities of telemedicine and medical IT are complementary and synergistic. Telemedicine is the use of information technology and electronic communication to deliver therapeutic services to patients who are in different locations [21]. The term telemedicine is closely related to this. The term is often used to include a wide range of applications of technology for distance learning, consumer work, and other applications that use electronic communications and information technology to support healthcare services. Telemedicine is not an independent specialist. Rather, it is a tool that can be used by healthcare providers to extend traditional medical practices beyond the walls of a typical clinic [22]. Additionally, telemedicine provides a novel way for people to maintain a healthy lifestyle, especially considering the COVID-19 pandemic [23]. It facilitates consumer participation in healthcare decision-making.
● Digital Health Knowledge Resources: It is a concept in which content is stored in digital format. A digital medical library collects and stores information in digital format and is accessible via a computer. In order to enhance, update, review, or analyse the delivery of healthcare, doctors, medical professionals, students, patients, consumers, and medical researchers can discover health and scientific information via digital health or medical libraries [24]. This has several advantages, such as one can access it anytime from anywhere if they have an internet connection, it needs little space for storage, and maintenance costs are much lower than traditional libraries. Digital libraries are user-friendly interface that provides clickable access to resources. To address the ever-growing number of electronic publications, we need to develop new tools and technologies that enable effective, automated semantic classification and search.
● Health and Hospital Information Systems: In this discipline, health information systems are the most contentious issue. Instead of using IT, the majority of national hospitals, especially public hospitals and healthcare facilities, use manual processes. The timely availability of patient records may have an impact on the quality of healthcare. The primary software application areas for information systems in modern healthcare organisations are now patient intake and enrolment. Medical record management, patient billing, general financial management, patient care divisions, outpatient management, decision support, management reporting, office automation, and specialised systems. In order to meet the needs of modern medicine, hospitals deploy automation.
● E-learning technologies and applications in Health Science: E-learning is the electronic transfer of skills and knowledge. E-gaining knowledge of programs and methods encompass web-primarily based totally gaining knowledge of, computer-primarily based totally gaining knowledge of. Content can be text, images, animations, streaming video, and audio in any format that can be delivered via the Internet, intranets/extranets, audio or videotapes, satellite television, and CD-ROMs.
● Biomedical informatics for biomedical research applications
● Medical Internet
● Virtual Reality and Simulation for Health
7. ICT AND HIT-BASED HEALTH PLATFORMS IN INDIA
● In accordance with the Integrated Illness Surveillance Program (IDSP), the Integrated Disease Surveillance Project (IDSP) Gateway enables reporting of disease surveillance data [25]. The National Health Mission (NHM), which includes the IDSP project, was launched in November 2004 and is presently in effect in all the Indian states and Union Territories. The main objectives of this plan are the decentralised lab-based, IT-enabled disease system management for illnesses that are prone to epidemics and the Rapid Response Teams' (RRT) identification and response to disease outbreaks. What it is, is the monitoring. On the IDSP site, you may access an epidemic signal dashboard to help you keep track of infections.
● Mother and Child Tracking System (MCTS): National Informatics Centre created this essential web tool, which was first released in 2009. (NIC). The Health and Family Department has launched this project to employ technology to offer children and pregnant women a variety of medical services. In order to register and follow expectant mothers and their children up to age 5, the MCTS Portal produces a 16-digit ID. Healthcare management can easily monitor the level of service with the help of this portal's user-friendly interface. Prenatal care, postpartum care, and vaccines are only a few of these services [26]. When a service is about to expire, the system can regularly send alerts to beneficiaries and medical professionals.
● The National Health Mission's eHMIS (electronic Health Management Information System) is a web-based digital project created to gather, combine, and analyse health-related data from the most remote medical facilities up to the national level. This facility-based aggregation solution facilitates quick data transmission from the facilities to the federal level and reduces errors in the flow process. Additionally, using your data is made easier by numerous visualisation tools, having a dashboard, and monitoring the data at all levels. Policymakers are helped in their decision-making process by the eHMIS tool for decision support [27].
● The National Vector Borne Disease Control Program created the NAMMIS (National Anti-Malaria Management Information System) as a web-based platform to track and frequently track the performance of malaria indicators [28]. The system was set up by medical specialists engaged in giving NVBPCP interventions, and it became fully operational in 2008.
● Digital Life Care: Digital Life Care is a web and Android-based platform developed by Dell [29]. Started as a pilot in Karnataka in 2014, it has been adapted to be deployed in all 29 states and Union Territory throughout India since late 2017. Digital Life Care was launched by Indian Minister Hon'ble Prime in April 2018. It is used in the public sector health sector across the country. Based on technology, this platform was developed to facilitate the screening and management of NCDs by midwives and physicians of assistant nurses, one of Ayushman Bharat Yojna's comprehensive primary care services. Midwives utilise iPads and the Android app to gather information out in the field. On the other side, physicians at primary, secondary, and tertiary levels in the healthcare system, together with dashboards, use the web platform. The effectiveness of health programmes can be checked by health authorities. ANMs and doctors are guided by prompts and videos in the module-based framework of Digital Life Care as they screen beneficiaries and offer referrals. The recipient examination, diagnosis, and follow-up regimen used by the Indian government is the foundation of this system.
● The PradhanMantriRashtriya Swasthya Suraksha Mission (PMRSSM), which is part of the Ayushman Bharat Yojna, was designed to be built within the context of the National Health Stack (NHS), however, the NHS goes beyond PMRSSM to carry different health industry sectors and of their branches to the government sector and both national and state-level support in the private sector [30]. The system seeks to establish a digital health record for every Indian, and upon successful registration with the National ID, a National Health Stack (NHS) ID, a special identification number for each inheritor, will be generated. The system intends to develop the biggest and most thorough database for the identification of fraud in relation to the creation of policies, medical insurance, health research, and other areas. This mechanism is crucial to the effort to achieve universal health insurance.
● National Health Policy: The National Health Policy, which was first adopted by the Indian Parliament in 1983 and then modified in 2002, endorsed the notion of integrating electronic communication media into the health sector [31]. According to the Ministry of Health and Family Welfare of the Government of India (2017) (Table 1), the role of digital health technology is emphasised as a crucial component of healthcare. The Aadhaar Card is used in this strategy to identify beneficiaries in a unique way, cellphones are used to gather real-time data, and it is integrated into the fiber-optic network of the nation (Fig. 3).
| Technology | Applications and Cons |
|---|---|
| Computerized physician order entry (COPE) | Reduce medication errors, not suitable for integrated CDS environment. |
| Clinical Decision Support (CDS) | Process improvement like automation, reminder, and clinical outcome predictions. |
| Barcode medication administration (BCMA) | Reduce errors in lab and medication. |
| Patient Data management systems (PDMS) | Reduce patient waiting time to meet doctor, better patient management. |
| Automated medication dispensing (ADC) | Reduce errors in intensive care units. |
| Retained surgical item detectors. | Retaining of the surgical items not be advised. |
| Patient portals | Improves patient-doctor relationships, reduces chart work, and makes data breaching possible. |
| Telemedicine - virtual visits | Possible to get treatment in any place, and all the peoples get treatment at the right time. |
| Telemedicine - Telemonitoring | Experts can guide juniors for the treatment for critically ill patients. Infrastructure is the main issue in this method. |
| Overall Electronic Medical Record EMR | Ultimate records for patients, making policies and security issues have been taken care. |
7.1. Introduction to Mobile Health
Medical treatment has been revolutionised by the integration of mobile health and sensor technologies, which also helps to avert potentially fatal circumstances. To solve the medical and technological issues and create efficient e-health systems, additional study is required. The identification of key problems in the current healthcare systems is aided by a thorough examination of global healthcare reports [32]. By boosting productivity and lowering healthcare expenditures, a well-functioning healthcare system enhances both individual health and a nation's economy [33]. We can improve patient care and promote economic growth by addressing these issues and putting creative ideas into practice.
Due to limited educational possibilities and a lack of health-related knowledge, financially strapped people typically have poorer access to health services and are more likely to engage in health-risk behaviours [34, 35]. Such situations are most common in poor nations when a lack of resources directly affects the systems. Therefore, there is an essential need to introduce unique methods of providing healthcare in these nations since doing so might greatly improve the general standard of the healthcare system and, as a result, the health of the people.
In order to monitor human behaviour, physiology, the environment, and interactions among these [36-38], MOBILE sensing, a paradigm for sensing, is used (Fig. 4). It makes use of the ubiquitous sensors incorporated into mobile devices, such as smartwatches and mobile phones. Numerous studies have looked at the application of mobile sensing devices in the areas of mental health and chronic care [39, 40]. Early futuristic publications [41, 42] suggested the basic framework of mobile health (mHealth) sensing approaches, which use “non-invasive” mobile sensing systems [43] to collect data for human activity recognition and infer the person's health state. For each key health issue discussed here, mHealth sensing draws from the perspectives of personalised medicine and public health [44]. Personalized Health: Personalized medicine is patient-centred, with treatments, procedures, interventions, and/or goods being personalized to each patient depending on their expected response or risk of developing disease [45]. As a result, the objective of personalized medicine is to enhance and maximize each patient's response to treatment by detecting, tracking, and forecasting their current state of health [46]. Public Health: A group of people's collective health results and how those outcomes are distributed among them are referred to as their population's health [47]. Promoting a target population's health is the aim of population health [48], whose methods include identifying health outcomes, comprehending patterns of health status, and formulating intervention strategies [49].

8. COVID ERA
In the panic era of COVID-19, several healthcare applications were developed that aid the monitoring of patients, and communication among patients, doctors and authorities. The National Informatics Centre (NIC) created the Aarogya Setu Data Access and Knowledge Sharing Protocol, and the Ministry of Electronics and Information Technology, Government of India (MeitY), is in charge of its implementation [50]. COVID-19 Quarantine Monitor is a mobile app developed by the Tamil Nadu State government [51], which is designed to gather information about the home quarantine adopted by the citizens conforming with the official guidelines.
To collect information about the previous treatments and clinical tests undergone in the recent past, MeitY launched a survey app called COVID-19 Feedback. It is a contact tracing mobile application built upon Bluetooth, which was developed aiming to reduce the risk of COVID spread among the public. Punjab Government developed Corona Virus Alert App (COVA) to disseminate information related to COVID to users [52]. It also helps the government to share government orders, advisory regulations, travel plans, curfew pass and curfew information. Goa Ministry of Health was developed as an automated self-diagnose tool in the breakdown of COVID [53]. Based on the information feed by the users, it notifies them about COVID Protocols like wearing masks, self-quarantine, social distancing, and available doctors and primary health centres nearby. Along with COVID-19, the pandemic has affected how other diseases are treated by disrupting healthcare systems and delaying the detection and treatment of disorders like cancer and chronic diseases. Other new infectious illnesses have emerged in recent years, including monkeypox, hepatitis A, RSV, and norovirus. These illnesses can be transmitted by coming into touch with sick individuals, their body fluids, tainted food, or tainted water. It is crucial to be knowledgeable about these illnesses and take precautions to avoid getting sick.
The implementation of policies to implement HIT has always been the focus of government attention, and a full-scale exploratory initiative is underway to study the coordination of national medical IT infrastructure and networks. However, the challenges of implementing HIT are:
● Government Funding: In order not to hesitate to adopt HIT in the government's medical field, the government's funding for HIT needs to be further improved. In addition, we need to ensure that the number of trained medical IT specialists is increased.
● Computer literacy: A high percentage of computer literacy among government officials, and mostly private providers, should be one of the government's main goals.
● Infrastructure and Coordination: Improving support infrastructure and coordination between the public and private sectors is important for the proper implementation of policies [54].
● Interoperability: The interoperability discussion focuses, among other things, on the development of content and messaging standards and on proper security and privacy protection. Interoperability needs to be achieved in rapidly growing applications in areas such as home telemedicine and remote patient and consumer monitoring.
● Information Overload: Healthcare IT or telemedicine is not a cure for the inadequacy associated with the healthcare system, nor is it intended to be a cure for HIT. In fact, too much information about wireless media, or too much information from a large number of patients to one doctor or a small group of doctors, can lead to over-information and inadequate corrective action.
CONCLUSION
In order to stop the epidemic controlling epidemics requires strong enabling environments as well as modern, digital health information systems. The on-going deployment and improvement of the HIS require sustainable financial resources and government backing. Promoting digital solutions is crucial even after the COVID-19 pandemic. The moment has come to talk about potential solutions to get timely, accurate, and trustworthy health data to guide policy decisions while upholding privacy rights and the highest standards of ethics. The function of health-related information technology in the Indian healthcare system is clarified in this article. IT also highlights the part played by government agencies in the creation of mobile and web apps to digitalize medical records and increase system dependability.
LIST OF ABBREVIATIONS
| HIT | = Health information technology |
| CAGR | = Compound annual growth rate |
| BGL | = Blood glucose level |
| ARLNA | = Association of record librarians of north america |
| ICT | = Information and communication technology |
| EHRs | = Electronic health records |
| IDSP | = Integrated disease surveillance project |
| NHM | = National health mission |
| RRT | = Rapid response teams |
| MCTS | = Mother and child tracking system |
| eHMIS | = Electronic health management information system |
| NAMMIS | = National anti-malaria management information system |
| COVA | = Corona virus alert |
ACKNOWLEDGEMENTS
Declared none.


